The fact that substance use is more common among adults with mental health issues makes sense when you consider addiction expert Jean Kilbourne’s words. “Addiction begins with the hope that something “out there” can instantly fill up the emptiness inside.”
On that note, how likely is it we are all addicted to something? Whether to food, sex, or drugs, status, money, or praise. Choosing to use our unhealthy habits to fill up our emptiness inside, to cover up our emotions. Choosing to numb out rather than reach out.
If that is the case, what would happen if we took time to dig deep to identify the cause of our emptiness, perhaps we could begin to heal. Absolving the desire to escape into our addictions and also resolving the internal turmoil of mental illness. Perhaps lowering the statistics of substance use we are seeing today.
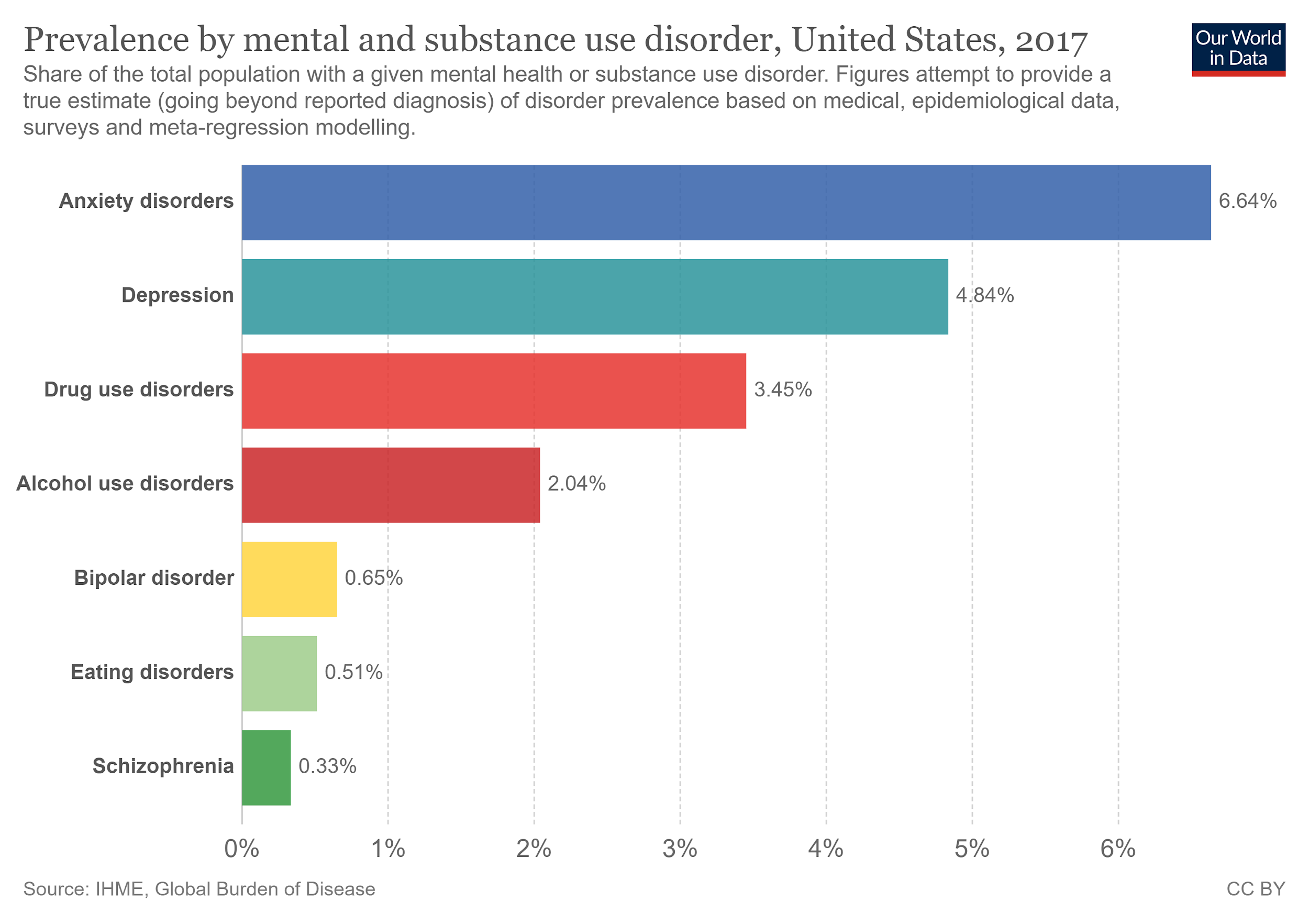
Mental illness continues to take the lead over substance abuse in the United States. [Image from Our World In Data.]
The data
Data from 2018 finds 57.8 million American adults are living with a mental and/or substance use disorder (SUD). Broken down further, 47.6 million have a mental illness, 19.3 million are facing substance abuse, and 9.2 million adults are living with both.
Among adolescents, at least 358,000 have a SUD together with depression. Numbers trending upward well before the pandemic. As mental health continues to take a major toll in the time of COVID-19, it seems logical to assume substance use disorders will also ascend.
Current results from the National Survey on Drug Use and Health (NSDUH), indicates rates of tobacco use double with mental illness, binge drinking is slightly higher yet, and rates of illicit drug use nearly triple.
So, is it the substance abuse that leads to mental illness? Or the mental illness that leads to substance abuse? The answer may be both.

Mental illness has a way of making one feel like life is always too much or never enough. Substance use disorders become one form of self medicating. [Photo by Daniel Reche from Pexels.]
The chicken or the egg.
While each individual is surely unique, certain substances, when abused, may cause symptoms of mental health disorders, such as feelings of depression or anxiety. In other cases, mental illness itself may push people to turn to substance abuse as a means of self-medication.
There is also evidence to suggest both mental illness and SUDs share common risk factors. Elements such as changes in brain composition, genetics, or childhood trauma, may increase likelihood for either diagnosis.
Evidence suggests, whether you have a mental illness or substance use disorder, or if they merely run in your family, you are already at higher risk for the other.

Family support is key to healthy recovery during treatment for substance use disorders. [Photo by Pixabay from Pexels.]
What can you do?
Research shows that family support can serve as a major factor in supporting a loved one with mental and substance use disorders. Not to mention, loved ones are most likely to notice something is awry, indicating an illness or disorder. That being said, helping a loved one with a mental or substance use disorder can be demanding, so caregivers must also prioritize their own self-care.
If you or a loved one is living with both mental illness and a substance use disorder, treatment must be sought out for each one.
Whatever treatment option you choose, we are here to help. Search our directory to find a treatment provider near you.